Since 1963, Cook Medical has been a champion of minimally invasive treatment options for patients. In the case of the centesis and drainage procedural areas, the healthcare industry discussion has largely centered around the efficacy of large-bore versus small-bore catheters.
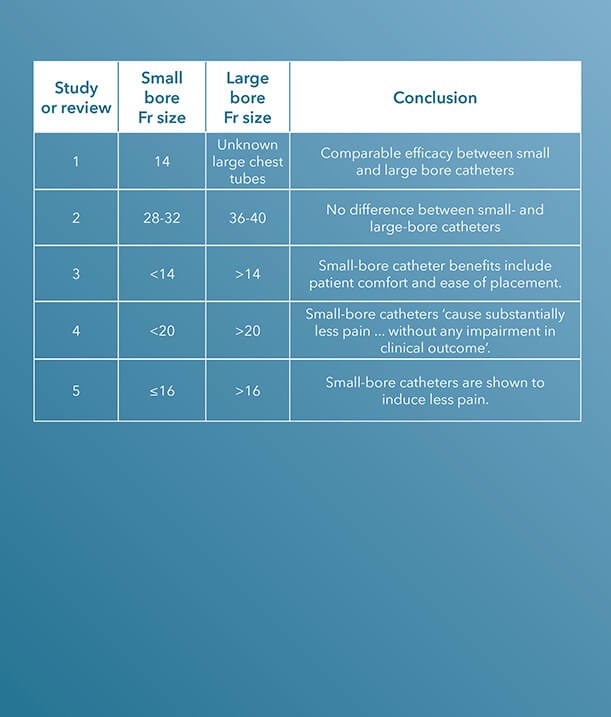
Within the last decade, there have been several clinical studies and review articles published in peer-reviewed journals stating the increased efficacy and improvement of small-bore catheters versus large-bore catheters for pleural and pericardial drainage procedures.
To see Critical Care’s entire product portfolio of small-bore chest tubes for pleural and pericardial drainage, click here.
ARTICLE 1 (STUDY)
“Two-year experience of using pigtail catheters to treat traumatic pneumothorax: a changing trend,” published in The Journal of Trauma in 2011, is a study comparing small-bore, 14 Fr pigtail catheters to chest tubes in patients with nontraumatic pneumothoraces.
A chest tube, “because of its large caliber and significant trauma during an insertion, can cause pain, prevent full lung expansion, and worsen pulmonary outcome. Pigtail catheters (PC)… are smaller and less invasive,” the introduction to the study states.¹
The charts of 9,624 trauma patients over a two-year period at a Level I trauma center were evaluated. The study concludes that the “demographics, tube days, need for mechanical ventilation, and insertion-related complications were similar,” using these characteristics to determine that pigtail catheters have a comparable efficacy to chest tubes.1
ARTICLE 2 (STUDY)
36 to 40 Fr chest tubes were also compared to small-bore pigtail catheters in a similar study also published in The Journal of Trauma and Acute Care Surgery, titled “Does size matter? A prospective analysis of 28-32 versus 36-40 French chest tube size in trauma.”
There was no difference in the efficacy of drainage [or] rate of complications.2
In this study, the authors claim that “the optimal chest tube size for the drainage of traumatic hemothoraces and pneumothoraces is unknown.”2 This study was designed to compare the efficacy of small-bore versus large-bore drainage catheters in patients with thoracic trauma.
Data were gathered on 293 patients who required open chest tube drainage within 12 hours of admission to a Level I trauma center.
“Clinical demographic data and outcomes including efficacy of drainage, complications, retained hemothoraces, residual pneumothoraces, need for additional tube insertion, video-assisted thoracoscopy, and thoracotomy were collected and analyzed by tube size,” the authors indicate.2 Small-bore catheters, ranging from 28 to 32 Fr, were compared with large chest tubes, ranging from 36 to 40 Fr; a total of 353 catheters, 186 small and 167 large, were placed during the study.
The authors determined that “the need for tube reinsertion, image-guided drainage, video-assisted thoracoscopy, and thoracotomy” are the same when comparing small-bore to large-bore catheters.2
“For injured patients with chest trauma, chest tube size did not impact the clinically relevant outcomes tested. There was no difference in the efficacy of drainage, rate of complications including retained hemothorax, need for additional tube drainage, or invasive procedures,” the study concludes.2
ARTICLE 3 (REVIEW)
In 2013, a paper published in Clinics in Chest Medicine aimed to generalize the use of small-bore catheters for drainage procedures, including in pleural infection.
In “Straightening out chest tubes: what size, what type, and when,” the authors state that “small-bore tubes (<14 Fr) are effective for most pleural processes. Various types of pneumothorax and malignant and infected complicated pleural effusions have been successfully managed with small-bore chest tubes.”3
Abundant literature supports a paradigm shift towards the more routine use of small-bore chest tubes for managing pleural disease.3
The authors also state that the benefits of using small-bore drainage catheters include patient comfort and ease of catheter placement.3
The study concludes that “abundant literature supports a paradigm shift towards the more routine use of small-bore chest tubes for managing pleural disease.”3
ARTICLE 4
A study published in CHEST, titled “The relationship between chest tube size and clinical outcome in pleural infection,” aimed to determine the optimal choice of drainage catheter sizes for pleural infection.
This multicenter study enrolled 405 patients and evaluated “the combined frequency of death and surgery, and secondary outcomes,” specifically “hospital stay, change in chest radiograph, and lung function at 3 months,” in patients who received a variety of sizes of chest tubes. In 128 of the 405 patients, a pain scale was also included.4
“There was no significant difference in the frequency with which patients either died or required thoracic surgery in patients receiving chest tubes of varying sizes,” the study notes; however, “pain scores were substantially higher in patients receiving (mainly blunt dissection inserted) larger tubes.”4
The study concludes that “smaller, guide-wire-inserted chest tubes cause substantially less pain than blunt-dissection-inserted larger tubes, without any impairment in clinical outcome in the treatment of pleural infection.”4
ARTICLE 5 (REVIEW)
Although the precise optimal chest drain size remains unknown, a review article titled “Optimal chest drain size: the rise of the small-bore pleural catheter,” published in Seminars in Respiratory and Critical Care Medicine, asserts that “objective data supporting the use of large-bore [chest] tubes is scarce.”5
The onus now is on those who favor large tubes to produce clinical data to justify the more invasive approach.5
In support of the efficacy of small-bore drains, the article states, “Increasing evidence shows that small-bore catheters induce less pain and are of comparable efficacy to large-bore tubes, including in the management of pleural infection, malignant effusion, and pneumothoraces. The onus now is on those who favor large tubes to produce clinical data to justify the more invasive approach.”5
Interested in chatting with a Cook Medical representative?
Please submit the required information to connect with your local Cook representative. This form is intended for US-based physicians only. Please see our Privacy Statement for data protection notices relating to our collection and use of your data.
2. Inaba K, Lustenberger T, Recinos G, et al. Does size matter? A prospective analysis of 28-32 versus 36-40 French chest tube size in trauma. J Trauma Acute Care Surg. 2012;72(2):422-427.
3. Mahmood K, Wahidi MM. Straightening out chest tubes: what size, what type, and when. Clin Chest Med. 2013;34(1):63-71.
4. Rahman NM, Maskell NA, Davies CW, et al. The relationship between chest tube size and clinical outcome in pleural infection. Chest. 2010;137(3):536-543.
5. Fysh ET, Smith NA, Lee YC. Optimal chest drain size: the rise of small-bore pleural catheter. Semin Respir Crit Care Med. 2010;31(6):760-768.