The results discussed in the following article were extracted from data obtained in April and May of 2020.
In the early months of onset, the COVID-19 pandemic forced significant changes and challenges upon healthcare industries around the world, affecting urological elective procedures for the treatment of lower urinary tract symptoms and procedures such as benign prostatic hyperplasia (BPH) surgery.
 An extraordinary impact
An extraordinary impact
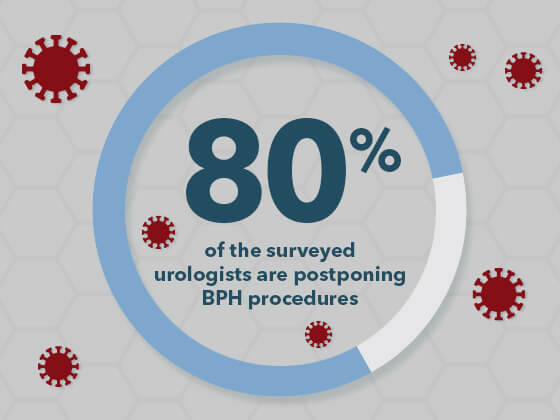
In a recent survey of 2,494 urologists from 76 countries, BPH was positioned as one of the lowest priorities of non-oncological procedures. This resulted in 80% of the surveyed urologists postponing BPH procedures until the pandemic is over.1 According to another study, approximately 2.5 million urological benign surgeries were estimated to be canceled during the peak of disruption by COVID-19. Consequently, after the pandemic, if countries increased their surgical volume by 20%, then it would take a median of 45 weeks to normalize the number of surgeries.2
Why a low priority?
Some of the top reasons for lowered priority of BPH treatments:
- Proposed COVID-19 guidelines – The World Health Organization (WHO) advised all elective surgeries to be postponed, therefore the impact of COVID-19 was greater for elective surgeries than non-elective surgeries. European Association of Urology (EAU) and American College of Surgeons (ACS) “guidelines recommend prioritising surgeries based on local resource availability,” which can vary with regional differences.1
- Risk of viral transmission – There is some risk of viral transmission with BPH endoscopic surgeries due to the presence of SARS-CoV-2 in blood, feces, and urine. Potential risk exists for splashing and aerosols during the procedure. Blood splashing on goggles is routinely underestimated risk. Blood splash events on eye protection occurs 33%–100% of the time, according to several studies.3
Any evacuations of irrigation fluid during any endourological procedure must be collected through a closed system to decrease risks. The EAU guidelines recommend only treating high-priority cases surgically during the COVID-19 pandemic. Treating low priority patients may increase the risk of unnecessary COVID-19 transmission.3 - Alternative treatments – COVID-19 ramifications in some parts of the world may not allow for certain adaptations to treatments. For example, the pandemic caused an 86% drop in “urological surgeries during the lockdown period” at a tertiary care, academic center in India, which was designated as a COVID-dedicated facility. Telemedicine, instead of physical outpatient visits, was “used for consultation and planning elective surgeries.”4 In one article, operations for BPH during the pandemic are not recommended, instead “if necessary, indwelling urinary catheter placement or percutaneous cystostomy with local anesthesia are indicated for preservation of renal function” even in cases with urinary retention.5
Regional comparisons
The survey of urologists also revealed distinctions in postponement of urological procedures in specific regions. “Follow-up examinations of the adjusted standardized residuals from the survey revealed that respondents from East/Southeast Asia consistently reported higher than expected rates of no change for all procedures.”1 “Among all the regions, Europe appears to be following the guidelines most closely. This region reported the highest rates of postponement of procedures categorised as low priority by guidelines and the lowest rate of postponement of procedures designated as high priority or urgent.”1
It should be noted that in some circumstances, changes in protocol allowed urologists to continue performing lower priority procedures. Cases that may have previously required in-patient facilities and overnight stays may have been referred to outpatient settings like ambulatory surgery centers in order to allow the patient time to recover in a non-COVID-19 environment with same-day discharge. For example, a holmium laser enucleation of the prostate may have been considered an overnight stay for a patient. With concerns of safety and available bed space, the treatment could move to an outpatient center with the patient discharging later that day with only a catheter remaining. “Surgical approach of BPH must be considered depending on availability of disposable material, infrastructure, and the epidemiological COVID-19 status of your area,”3 as well as safety considerations for the patient and staff.
COVID-19 has dramatically impacted the volume and treatment options for physicians globally. Whether these changes become standard practice once the pandemic subsides remains in question; however, new doors have opened for laser treatment for patients with BPH. Laser treatment can easily be adopted by additional surgery centers and other outpatient facilities not focused on COVID-19 patients. To meet the growing need, Cook Medical offers a breadth of urological devices from low-watt holmium lasers with the functionality of higher-watt lasers to the higher-watt holmium and thulium lasers.
Research shows us that physicians are adapting to the COVID-19 environment with changes in treatment methods for BPH or postponement of procedures. How have your treatment philosophies changed in the COVID-19 era? Join the conversation on Twitter #CovidBPHTreatment.
- Gravas S, Fournier G, Oya M, et al. Prioritising urological surgery in the COVID-19 era: a global reflection on guidelines. Eur Urol Focus. 2020;6(5):1104–1110.
- COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;10.1002/bjs.11746.
- Pinto AMA, González MS. Endourology and benign prostatic hyperplasia in COVID-19 pandemic. Int Braz J Urol. 2020;46(Suppl 1):34–38.
- Devana SK, Chaudhary K, Sharma AP, et al. Changing urological practice during COVID-19. Indian J Urol. 2020;36(3):153–158.
- Carneiro A, Wroclawski ML, Nahar B, et al. Impact of the COVID-19 pandemic on the urologist’s clinical practice in Brazil: a managment guideline proposal for low- and middle-income countries during the crisis period. Int Braz J Urol. 2020;46(4):501–510.